TMS Therapy Shows Potential in Addressing Autism Symptoms
Autism spectrum disorder (ASD), a neurodevelopmental condition, affects approximately 1 in 36 children, with diagnosis rates notably higher in boys. Similar to ADHD, many girls remain underdiagnosed due to different symptom presentations or social masking, which can delay intervention. Autism is marked by difficulties in social communication, along with restricted and repetitive behaviors, as defined in the DSM-5. While symptoms often appear early, milder forms may remain unnoticed for years.
Understanding Neural Rigidity in Autism
Research indicates that individuals with ASD struggle with neural flexibility—the brain’s ability to shift between states. This “rigidity” is linked to reduced connectivity in key networks such as the frontoparietal network (FPN) and the left prefrontal cortex. These brain dynamics show functional segregation, where systems don’t integrate well, contributing to cognitive inflexibility.
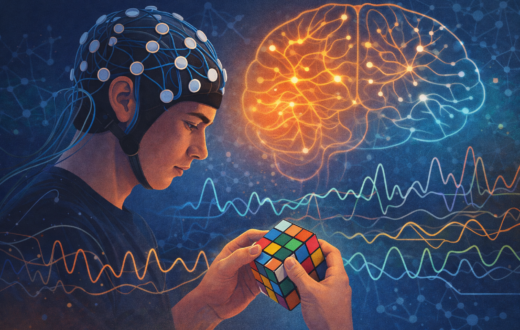
Transcranial Magnetic Stimulation (TMS) as a Tool for Flexibility
A new study in Nature Neuroscience (2025) by Watanabe & Yamasue explored the use of transcranial magnetic stimulation (TMS), a non-invasive brain stimulation method, guided by real-time EEG in a technique called brain state-driven neural stimulation (BDNS). By targeting the right parietal lobule, a brain region responsible for spatial and sensory integration, they aimed to reduce neural rigidity.
TMS, already FDA-approved for depression and OCD, uses magnetic pulses to activate neurons. In this study, the stimulation was timed to occur precisely when brain networks showed low connectivity, making the intervention both targeted and adaptive.
Study Design and Findings
Involving 50 ASD participants and 50 neurotypical controls, researchers assessed three core domains:
- Cognitive flexibility (via spontaneous task-switching)
- Perceptual flexibility (via bistable images like duck-rabbit illusions)
- Social perception (via a friend-or-foe nonverbal test)
Using EEG and later confirmed by resting-state MRI, they identified four distinct brain states, noting that participants with ASD had more difficulty transitioning between these states. Applying BDNS enhanced transitions, especially from major brain state 1, by increasing indirect transitions through minor states.
Clinical Improvements
A follow-up 12-week TMS trial with weekly sessions showed:
- Neural rigidity and cognitive flexibility improved by week 1
- Perceptual flexibility improved by week 7
- Social information processing improved by week 9
Connectivity within the FPN, visual network (VN) and salience network (SN) played a key role, especially when the default mode network (DMN) was active and FPN inactive.
Future of Autism Treatment
This personalized use of TMS with EEG monitoring offers a new avenue for precision neurotherapy in autism. While the study is small, it provides proof-of-concept for using brain-state-responsive interventions. Further research may allow for individualized protocols tailored to specific dysconnectivity profiles, potentially combined with behavioral therapies.